ADVERTISEMENT
A Comparison of Collagenase to Hydrogel Dressings in Wound Debridement
Abstract:
Comparisons of collagenase to other methods of debridement, including wet to dry dressings, have been reported in the literature; however, studies comparing collagenase to hydrogel have not been reported. Objective. Time to complete necrotic tissue debridement with collagenase compared to hydrogel in institutionalized adults with pressure ulcers. Methods. Randomization occurred after obtaining informed consent to avoid selection bias. Subjects received daily dressing changes with either hydrogel or collagenase followed by a standard semi-occlusive dressing to evaluate time to debridement up to Day 42. Investigators, who were blinded to randomization, evaluated weekly wound photographs for necrotic tissue debridement and wound healing parameters using a digital planimetry software package. Nonviable tissue was not cross-hatched in either group. Results. Twenty-seven nursing home residents were enrolled over a period of 1 year. According to a Student’s t test, there were no significant differences between groups for age, gender, age of wound, or percentage of nonviable tissue at the time of enrollment (P = .03). Using a Pearson Chi square analysis, the collagenase group was found to have statistical (P = .003) significance in achieving full debridement by Day 42. Conclusion. This study showed statistical significance in favor of collagenase when used to debride nonviable tissue in pressure ulcers. Despite recommendations to cross-hatch eschar, statistical significance was still achieved when wounds were not cross-hatched, indicating clinical utility in settings without clinician availability for the cross-hatching procedure. Wound bed preparation (WBP) continues to be an essential component of chronic wound management. By addressing the relationship between necrotic tissues, exudate, bacterial and cellular dysfunction, an optimal wound healing environment can be achieved.1 The goal of debridement, integral to the WBP concept, is to remove necrotic tissue. Methods to achieve debridement include complete surgical excision, bedside sharp debridement, chemical/enzymatic/biological and autolytic agents, as well as mechanical agents. The choice of debridement methods depends upon the clinician, who considers wound characteristics and other local assessment findings, patient comorbidities, the time frame needed to achieve debridement, and the available skills and resources to safely manage the debridement process in the particular clinical setting. With the exception of surgical debridement, complete debridement of necrotic tissue in one patient encounter is a rarity.1 In nonspecialized outpatient, long-term care, and homecare settings, availability of a skilled clinician to provide bedside sharp debridement is very limited. Consequently, the use of chemical and autolytic debriding agents has been the primary method to achieve this aspect of WBP. Numerous studies have previously shown the debridement efficacy of chemical/enzymatic/biological agents when compared to wet-to-dry dressings.2 Wet-to-dry dressings are no longer considered standard of care, and there has been a shift in the literature that compares topical wound care therapies to moist wound care using hydrogel. No published studies have re-examined the efficacy of chemical/enzymatic/biological debriding agents to hydrogel in pressure ulcers. Enzymatic and autolytic debridement is frequently used in the long-term care setting as a simple, safe, and practical method to achieve the removal of nonviable tissue in the population served by these facilities. It can be used as either a short term conservative approach while arranging for surgical/sharp debridement3 or as a longer term strategy, as long as the wound bed parameters are improving.3 Initial debridement, defined as “the removal of necrotic, damaged, and/or infected tissue”3 differs from “maintenance debridement,” which is a process that not only frees the wound bed from obstacles to healing, but offers a continuous and active debridement of that wound bed. These obstacles include the persistence of cellular debris, uncontrolled matrix metalloproteases, and bacterial bioburden. The aim of this study was to compare collagenase to hydrogel for initial debridement and promotion of maintenance debridement. This was a two-phase study comparing collagenase to hydrogel. Phase 1 evaluated time to complete wound debridement and Phase 2 evaluated time to complete wound healing. It is important to note that only Phase 1—time to complete debridement—is reported in this manuscript. 
Methods
The local Institutional Review Boards of the long-term care facilities from which patients were recruited approved the study protocol. Patients or their legal representative were asked to provide written informed consent. Inclusion and exclusion criteria are listed in Table 1. The primary outcome of the initial phase of this evaluation was to determine number of days needed to achieve complete debridement. Patients that were unable to achieve this primary endpoint by Day 42 were then removed from the study in order to receive other methods of debridement. Randomization occurred after informed consent was obtained to reduce selection bias. Patients were assigned to either the collagenase group (Santyl® Ointment, Healthpoint, LTD., Fort Worth, TX) or hydrogel (SoloSite™ Gel, Smith & Nephew, Largo, FL). Following initial assessment, the wounds were irrigated with normal saline using a device that delivered 4–15 psi (Irrimax®, Weston, FL) and wound photographs were taken. Both the PUSH Tool score Version 3.04 and the Wound Bed Score (WBS)5 were calculated at the initial evaluation and on Day 42. Both of these tools have been tested for clinical validity and reliability to monitor wound healing status over time. The PUSH Tool was initially developed specifically for pressure ulcers. Within this rating system, lowering scores signify wound improvement. Conversely, increasing scores on the WBS tool indicate wound improvement. The initial evaluation and application of the assigned agent was completed by the same investigator (CM) and repeated weekly along with wound photos. Cross-hatching, the recommended procedure for collagenase6 application, which consists of scoring of nonviable tissue using a #10 blade to expose more surface area for drug exposure, was not done for either agent as to replicate common clinical practice in the long-term care setting. Each dressing change consisted of normal saline irrigation followed by application of the assigned therapeutic agent (nickel thick) to the entire wound bed. The wound was then covered with a semi-occlusive dressing (COVRSITE™, Smith & Nephew, Largo, FL). The nursing staff at the long-term care facility performed daily dressing changes and as needed if the dressing integrity was lost. Loss of dressing integrity was defined as soiling with fecal or urinary incontinence or inadvertent removal of the dressing as to expose the wound. The investigator trained all nursing staff at the facility. In the presence of wound depth, after application of the assigned agent, the wound was then filled to the depth equal to that of the surrounding wound tissue with gauze dampened with normal saline so that there was no excess moisture noted when pressure from the clinician’s hand was applied. This was also covered with a semi-occlusive dressing (COVRSITE). 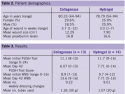 Two designated Investigators (AOC, ML), blinded to the assigned randomization group, evaluated photos for the percentage reduction of nonviable tissue and wound healing parameters using calibrated digital wound measurement software (PictZar®, BioVisual Technologies, Elmwood Park, NJ). Collagenase subjects did not have cross-hatching of any necrotic tissue, as this modality is frequently unavailable in the long-term care setting. The absence of cross-hatching the nonviable tissue simulates actual practice in this type of clinical setting. Sharp debridement was not performed at any visit.
Two designated Investigators (AOC, ML), blinded to the assigned randomization group, evaluated photos for the percentage reduction of nonviable tissue and wound healing parameters using calibrated digital wound measurement software (PictZar®, BioVisual Technologies, Elmwood Park, NJ). Collagenase subjects did not have cross-hatching of any necrotic tissue, as this modality is frequently unavailable in the long-term care setting. The absence of cross-hatching the nonviable tissue simulates actual practice in this type of clinical setting. Sharp debridement was not performed at any visit.
Results
Forty-two (42) patients were approached and 27 subjects consented to participate. Enrollment occurred over a 1-year period. Thirteen (13) patients were randomized to the collagenase group and 14 were randomized to the hydrogel group. Data analysis was performed by SPSS, (version 11.0.0), a statistical software package. Using Student’s t test, there were no significant differences in groups for age, gender, age of wound, or percentage of nonviable tissue at the time of enrollment (P < .03). More than half of the pressure ulcers (55.5%) were related to devices such as splints, braces, ill-fitting wheelchair armrests, or prosthesis. Wound size was statistically different; overall, the collagenase group presented with larger wounds (P < .004). Tables 2 and 3 provide a complete description of patient characteristics. Twenty-seven (27) patients completed Phase I up to Day 42 or full debridement, whichever occurred first. One patient developed wound deterioration and cellulitis at the wound site and was then removed from the study on Day 28, but had complete debridement prior to this episode, and thus data from this patient was included in analysis. In this study, the ability of collagenase to fully debride nonviable tissue in pressure ulcers within 42 days was superior to hydrogel as 11 (85%) of the 13 patients randomized to this modality achieved complete debridement within 42 days. In the hydrogel group, only 4 (29%) of 14 achieved this goal. Using a Pearson-Chi square analysis, the collagenase group was found to have statistical significance (P < .003) in achieving full debridement by Day 42. Reduction of nonviable tissue was greater on a weekly basis with the collagenase group as compared to the hydrogel group (P < .002). Overall wound size decreased faster (P < .009) in the collagenase group as compared to the hydrogel group.
Discussion
The primary aim of Phase 1 of this study was to compare collagenase to hydrogel for ability to debride nonviable tissue in pressure ulcers. Phase 2 of the study compared collagenase to hydrogel regarding the ability to provide maintenance debridement and promote full wound healing, and will be reported when fully completed; only Phase 1 is discussed here. Currently, collagenase is the only enzymatic debriding agent approved by the United States Food and Drug Administration (FDA) for the removal of nonviable tissue in the United States. Papain-urea agents were removed from the market voluntarily in 2008 as the FDA expressed concerns that the use of these agents in latex allergic patients may result in cross-reactivity with papain. Prior to 2008, papain-urea agents were the more frequently used enzymatic debriding agents. As such, clinicians who use enzymatic debriding agents in their armamentarium have had to increasingly rely on collagenase or the use of autolytic debridement, such as hydrogel. Evidence-based practice has supported both of these methods to achieve initial debridement in certain clinical situations.7 Hydrogels, which are composed of hydrophilic polymers in a dimensional matrix, act to facilitate removal of nonviable tissues.8 By creating an optimal moist wound bed environment, the body’s native enzymes are then able to work efficiently to breakdown necrotic tissue.8 Intrinsic enzymes are selective in the protein degradation. This passive method of debridement has been shown to be slow and associated with anaerobic bacteria.9 The hydrophilic components and water content of hydrogels vary, making general comparisons between this class of topical wound treatment and other, nonhydrogel, treatments difficult.10 However, hydrogels have been shown to be superior to moist saline gauze dressings.11 Bale et al12 compared two amorphous hydrogels and found little difference in time to debridement between them. Collagenase ointment, a metalloproteinase made from the bacteria Clostridium histolyticum, has been studied extensively with regards to its chemical and biological ability to degrade eschar. Denatured collagen is 75% of the dry weight of the skin.13 Pressure ulcer eschar has been shown to be composed of keratins, collagen, fibrin, elastin, fat, and proteogylcans.14,15 Eschar is anchored by collagen fibrils in the base of the wound.15 Shi et al16 examined collagenase selectivity and found that this agent has a high affinity for cleaving peptide bonds associated with type I collagen. This characteristic is viewed as favorable as its selectivity avoids the degradation of other proteins observed in the wound bed, such as growth factors. Intact collagen, surrounded in mucopolysaccharide casings, is minimally affected.17 Cross-hatching of the eschar using a #10 blade is recommended by the manufacturer to expose the collagen fibrils at the base of the wound to allow the medication to act as intended. In the long-term care setting, this practice is not routinely employed due to lack of skilled personnel to perform this function. Gray and Ramundo examined the literature comparing collagenase to other modalities for debridement.18 Collagenase was found to be a more rapid means of debridement as compared to placebo ointment or silver sulfadiazine. Mosher et al19 compared collagenase and hydrogel debridement in a nonexperimental design study using computer modeling, a decision analysis methodology and a Delphi consensus process with an independent panel of nine experts in geriatrics determined that the probability of achieving complete debridement of nonviable tissue in new full-thickness pressure ulcers was 70% within 2 weeks for those treated with collagenase versus 50% with hydrogel.19 Phase 1 represents the first study to compare collagenase to hydrogel for initial debridement of nonviable tissue in pressure ulcers in a clinical setting. Using descriptive statistics, the percent debridement within each group is similar to the Mosher et al predictive model. Despite recommendations to cross-hatch eschar, statistical significance was still achieved when wounds were not cross-hatched, indicating clinical utility in settings without clinician availability for this routine procedure. Limitations of this current study include the small number of enrolled patients, though the strong statistical differences between the two similar groups regarding debridement suggests that larger enrollment numbers would not produce markedly different results. These results cannot be generalized to all hydrogels owing to their different chemical compositions. Generalizations cannot be made in populations with wounds caused by other etiologies or outside the long-term care setting.
Conclusion
Pressure ulcers continue to be a challenging issue for clinicians in the long-term care setting. In addition to a frail population, the skill level of staff in conjunction with scope of practice issues, and the lack of availability of a skilled wound care practitioner on a daily basis add to the complexity in treatment decision making. It is no surprise that both autolytic and enzymatic debridement is frequently used as an initial debridement method. This study adds to the evidence base that enzymatic debridement has greater efficacy in the debridement of nonviable tissue in pressure ulcers as compared to hydrogel.
References
1. Vowden K, Vowden P. Wound bed preparation. World Wide Wounds. Available at: https://www.worldwidewounds.com/2002/april/Vowden/Wound-Bed-Preparation.html. Accessed: February 23, 2010. 2. Moore J, Jensen P. Assessing the role and impact of enzymatic debridement. Podiatry Today. 2004;17(7):54–61. 3. Falanga V, Brem H, Ennis WJ, Wolcott R, Gould, LJ, Ayello EA. Maintenance debridement in the treatment of difficult-to-heal chronic wounds. Ostomy Wound Manage. 2008;54(6 Suppl 1):S1–S13. 4. National Pressure Ulcer Advisory Panel (NPUAP). PUSH tool 3.0. Available at: www.npuap.org/PDF/push3.pdf. Accessed: February 23, 2010. 5. Falanga V, Saap LJ, Ozonoff A. Wound bed score and its correlation with healing of chronic wounds. Dermatol Ther. 2006;19(6):383–390. 6. Collagenase Santyl [package insert]. Fort Worth, TX: Healthpoint, Ltd; 2009. 7. Panuncialman J, Falanga V. The science of wound bed preparation. Clin Plast SurgM. 2007;34(4):621–632. 8. Turner T. The development of wound management products. In: Krasner DL, Rodeheaver GT, Sibbald RG, eds. Chronic Wound Care: A Clinical Source Book for Healthcare Professionals. 3rd ed. Wayne, PA: HMP Communications; 2001:293–311. 9. Dolynchuk KN. Debridement. In: Krasner DL, Rodeheaver GT, Sibbald RG, eds. Chronic Wound Care: A Clinical Source Book for Healthcare Professionals. 3rd ed. Wayne, PA: HMP Communications; 2001:385–390. 10. Eisenbud D, Hunter H, Kessler L, Zulkowski K. Hydrogel wound dressings: where do we stand in 2003? Ostomy Wound Manage. 2003;49(10):52–57. 11. Edwards J, Stapley S. Debridement of diabetic foot ulcers. Cochrane Database Syst Rev. 2010;20(1)1:CD003556. 12. Bale S, Banks V, Haglestein S, Harding KG. A comparison of two amorphous hydrogels in the debridement of pressure sores. J Wound Care. 1998;7(2):65–68. 13. Thomas AM, Harding KG, Moore KG. The structure and composition of chronic wound eschar. J Wound Care. 1999;8(6):285–287. 14. Alvarez O. Chemical debridement of pressure ulcers: a prospective, randomized, comparative trial of collagenase and papain/urea formulations. WOUNDS. 2000;12(2):293–301. 15. Ayello EA, Cuddigan JE. Debridement: controlling the necrotic/cellular burden. Adv Skin Wound Care. 2004;17(2):66–75. 16. Shi L, Carson D. Collagenase Santyl ointment: a selective agent for wound debridement. J Wound Ostomy Continence Nurs. 2009;36(6 Suppl 1):S12–S16. 17. Woodin AM. The corneal mucopolysaccharide. Biochem J. 1952;51(3):319–330. 18. Ramundo J, Gray M. Collagenase for enzymatic debridement: a systematic review. J Wound Ostomy Continence Nurs. 2009;36(6 Suppl 1):S4–S11. 19. Mosher BA, Cuddigan J, Thomas DR, Boudreau DM. Outcomes of 4 methods of debridement using a decision analysis methodology. Adv Skin Wound Care. 1999;12(2):81–88.
Address correspondence to:
Catherine T. Milne PO Box 1535 Bristol, CT 06011-1535 Email: ccna2@juno.com Phone: 860-340-8280
Disclosures:
Ms. Milne has received speaker honoraria from Healthpoint. The authors received unrestricted grants from Healthpoint.

















